11 February 2017
DNA Vaccine Delivery for Lassa Virus
Geneva researchers are collaborating with Inovio Pharmaceuticals to develop a way to improve DNA vaccine delivery for Lassa fever.
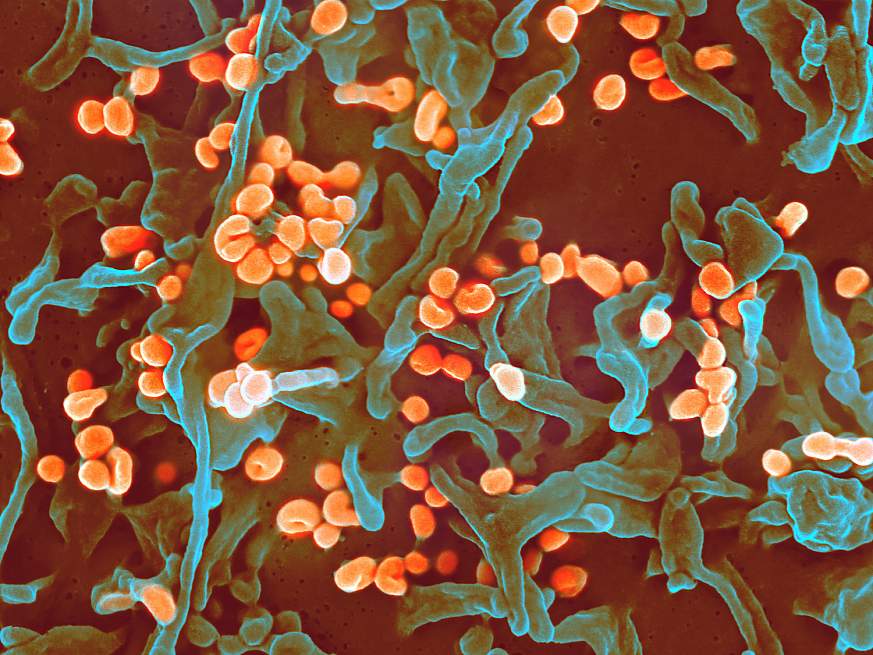
The Lassa virus causes a severe viral hemorrhagic fever that often presents itself alongside the Ebola virus. Those infected with Lassa virus experience respiratory distress, vomiting, facial swelling, chest pain, tremors, and brain inflammation. Lassa fever can be up to 20-50% fatal in humans and causes permanent hearing loss in about one-third of those who survive. The number of Lassa virus infections per year in West Africa is estimated at 100,000 to 300,000, with approximately 5,000 deaths.
The development of a vaccine to combat infectious diseases such as Lassa fever is necessary and is likely to have more success in the form of a DNA vaccine. When the modified DNA of a virus is used in a vaccine, the expression of the target genes results in the subjects’ immune system responding in a protective manner against the virus. While progress has been made in the creation and manufacturing of a DNA vaccine for Lassa fever, routine usage has been historically hindered due to ineffective delivery models. Delivering the Lassa DNA vaccine intramuscularly, directly into the muscle, a current method of vaccine delivery, has the potential to protect those infected from death, but preliminary studies show that it does not prevent fevers and viremia, a condition that causes measurable levels of the virus in blood samples.
Geneva researchers Dr. Connie Schmaljohn, Senior Research Scientist and Dr. Kathleen Cashman, Co-Investigator at the U.S. Army Medical Research Institute of Infectious Diseases, in collaboration with Dr. Kate Broderick, Senior Director of Research and Development at Inovio Pharmaceuticals, are developing a way to improve DNA vaccine delivery for Lassa fever through the use of an intradermal electroporation (ID-EP) device. The ID-EP device delivers an electric pulse to increase the uptake of the vaccine delivered under the skin, allowing for the vaccine to enter cells more effectively and resulting in an enhanced immune response.
The use of the ID-EP device is painless for subjects as it only penetrates the surface of the skin and uses an extremely low level of voltage, making it especially appealing for use in pediatric and geriatric populations. Additionally, unlike other current delivery methods, the use of the ID-EP device increases the efficacy of the vaccine by not only protecting those infected from death, but also by preventing viremia, meaning that the vaccine and dermal electroporation delivery will prevent secondary spread of the virus to close contacts.
The development of the ID-EP device in conjunction with a Lassa DNA vaccine has the potential to provide an effective response to Lassa virus as well as other biological health threats worldwide. With further developments, the hope is to apply similar methods in the delivery of vaccines for other infectious diseases, HIV, and cancer.