17 August 2021
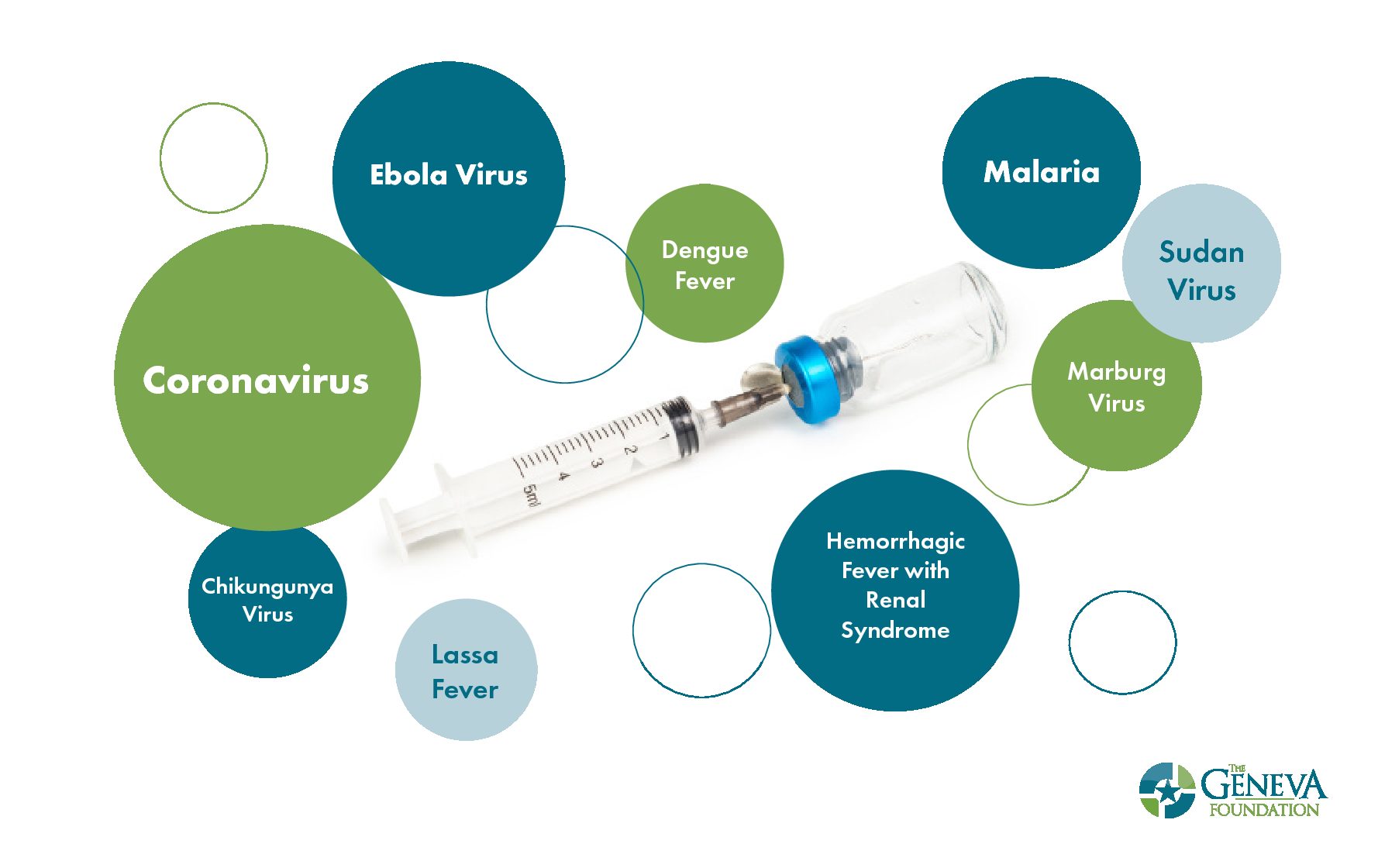
Vaccine Development: Coronavirus and 8 Other Infectious Diseases We’d Like to Eradicate
Vaccines are one of the most effective tools in protecting humans from infectious diseases globally and the only health intervention capable of eradicating a disease altogether. COVID-19 has demonstrated the severity, complexity, and globalization of infectious disease outbreaks and the need for vaccines.
The Geneva Foundation is proud to collaborate on infectious diseases research at leading federal laboratories and military treatment facilities including the Centers for Disease Control (CDC), National Institute of Allergy and Infectious Diseases (NIAID), U.S. Army Medical Research Institute for Infectious Diseases (USAMRIID), Walter Reed Army Institute of Research (WRAIR), Armed Forces Research Institute of Medical Sciences (AFRIMS).
Geneva’s scientific and technical program management expertise, along with our proven track record in infectious diseases research, has positioned our research teams as leaders in global infectious diseases with advancements in vaccine development. Here are eight life-threatening infectious diseases on our radar:
1. COVID-19
In 2020, while the world confronted a global pandemic, Geneva-funded researchers took on the additive mission of supporting the national effort to combat the deadly, novel coronavirus. Working with USAMRIID and CEPI, researchers early on in the pandemic set up animal laboratories for coronavirus vaccine testing, a key step in getting vaccines into humans. In August 2020, Geneva was selected by prime Pharm-Olam and the Department of Defense (DoD) to support Phase 3 clinical trials for two vaccine candidates under Operation Warp Speed (OWS). The availability of COVID-19 vaccines has undoubtedly saved lives.
Researchers are now conducting an observational study involving active duty service members who have received COVID-19 vaccines to assess vaccine protection against SARS-CoV-2 infection, including emerging variants. The Vaccine Effectiveness and Immune Response of SARS-CoV-2 Vaccines in Active Military Personnel study is led by Air Force Col. (Dr.) Jason F. Okulicz, an infectious disease physician and principal investigator at Brooke Army Medical Center at Fort Sam Houston.
2. Ebola virus
Ebola virus is a lethal disease found mainly in sub-Saharan Africa and is transmissible through direct contact with an infected animal or an infected person’s bodily fluids. The most recent outbreak was in February 2021 in the Democratic Republic of the Congo where 23 people were infected, resulting in 12 deaths.
Geneva’s 2016 Researcher of the Year John Dye, PhD, Chief of Viral Immunology at USAMRIID, is on the cutting edge of research and development of medical countermeasures against filoviruses, including Ebola virus, Sudan virus, and Marburg virus. Dr. Dye’s research tracks the immune response of Ebola virus survivors over time to determine an “immune profile” to drive future vaccine and therapeutic developments. His findings have driven protein-specific medical countermeasures against both viruses.
In December 2019, Geneva Senior Scientist Amy Shurtleff, PhD, a principal investigator at USAMRIID, led a research team in the development of the first vaccine to prevent Ebola, called Ervebo, which is now approved for human use.
3. Chikunhunya virus
The emerging global virus chikungunya is spread by the bite of an infected mosquito. It is a major concern for the U.S. military due to its capability to rapidly incapacitate people and cause debilitating chronic joint inflammation.
Dr. Dye and his team at USAMRIID recently discovered that two host proteins, named AAK1 and GAK, are critical for the lifecycle of multiple viruses, including dengue, chikungunya, and Ebola. His Geneva-managed research aims to optimize novel inhibitors that selectively inhibit AAK1 and/or GAK and that have already demonstrated promise against dengue virus, and advance their development towards a near-clinical stage product. This approach would also protect against multiple other biothreat agents, including chikungunya virus and ebola virus.
Damon Ellison, PhD, Chief of Bacteriophage Therapeutics at WRAIR, is part of a research collaboration evaluating an investigational live recombinant measles-vectored chikungunya vaccine in previously exposed adults. The Phase 2 clinical trial began in July 2019 with 21- to 50-year old subjects enrolled, followed by subjects aged 51 to 65 pending a review of favorable safety data.
4. Lassa fever
Lassa fever, an acute viral illness spread by infected rats, occurs most frequently in West Africa where over 300,000 people are infected annually resulting in approximately 5,000 deaths. This virus causes large, recurrent outbreaks with high case fatality rates and side effects with terrible impacts on the lives of the survivors, such as complete deafness.
In the hopeful culmination of 15 years of research, Geneva Principal Investigator Kathleen Cashman, PhD, in collaboration with Inovio Pharmaceuticals, is working to translate the DNA-based vaccine candidate INO-4500 into an FDA-approved vaccine for protection against Lassa fever.
5. Sudan virus
Sudan virus is one of six known viruses within the genus Ebolavirus and has caused eight confirmed outbreaks in African countries, which resulted in 412 deaths. One of the most recent outbreaks of the Sudan virus occurred in Uganda, where more than 450 people were infected, with about half resulting in deaths.
Dr. Dye and Geneva Principal Investigator Dr. Andrew Herbert’s team created an antibody cocktail that both neutralizes the Sudan virus and prevents it from entering cells. While not a vaccine, this cocktail, called RIID-F6H2, provides proof of concept for an antibody cocktail for Sudan virus that can move to advanced development for the consideration of human treatment. This is in addition to other Sudan virus vaccine development work being conducted at USAMRIID.
6. Dengue fever
Dengue outbreaks are spread to people through the bite of an infected Aedes species mosquito. Dengue is common in more than 100 countries around the world. Forty percent of the world’s population live in areas with a risk of dengue. The establishment of the U.S. Africa Command in 2007 means that U.S. service members are at continuous risk of acquiring filovirus infections, including dengue, while on duty.
Recently, Dr. Damon Ellison published results of an evaluation of the extended efficacy of Dengvaxia, the world’s first dengue vaccine introduced by Sanofi Pasteur in 2019. Dengvaxia is approved by the FDA for use in children ages 9-16 living in areas where dengue is common (U.S. territories of American Samona, Puerto Rico, and the U.S. Virgin Islands. Results in the manuscript demonstrated that “Cumulative vaccine efficacy was positive for both subclinical and symptomatic infection, although the protective effect of the vaccine was concentrated in the first 3 years following vaccination.”
7. Malaria
Malaria, a mosquito-borne disease, infects approximately 228 million people with approximately 405,000 deaths annually. The majority of infections are children under the age of five. Individuals with malaria often experience fever, chills, and flu-like illness. Left untreated, they may develop severe complications and die. Infection from malaria is responsible for millions per year in associated evacuation and medical care costs to the U.S. military.
In 2007, Geneva supported the first international study on the development of a malaria vaccine at AFRIMS in Thailand. Since that time, Geneva has proudly helped military researchers at laboratories such as WRAIR in the pursuit of a malaria vaccine. Despite the discovery of several malaria candidate vaccine antigens, there is currently no highly efficacious malaria subunit vaccine. Researchers are hopeful that advances in adjuvant and/or vaccine delivery methods will produce more efficacious malaria vaccines and overcome drug resistance to currently available antimalarials.
8. Marburg virus
It is unknown how Marburg virus first transmits from its animal host to humans; however, a connection has been made to those who have prolonged exposure to mines or caves inhabited by the African fruit bat. Once infected, it can spread via direct contact with others and carries a fatality rate of up to 88%.
Geneva, along with USAMRIID, Exxell Bio, and Thomas Jefferson University, received an award in 2017 from NIAID, to develop and test the first vaccine to induce protection against four hemorrhagic fever viruses (Ebola, Sudan, Marburg, and Lassa fever) which can damage blood vessels, cause internal bleeding and result in high mortality rates. The research aim is to create a broad scope of coverage with a tetravalent vaccine – one that covers four of these deadly viral diseases. This study has a potential completion date of July 2025.
9. Hemorrhagic Fever with Renal Syndrome
Hantaviruses are carried by infected rodents and transmitted by exposure to rodent excreta and found throughout the world. At least four Hantaviruses are known to cause thousands of cases of hemorrhagic fever with renal syndrome (HFRS) each year. Symptoms of HFRS include intense headaches, back, and abdominal pain, fever, chills, nausea, and blurred vision and can progress to acute shock, and kidney failure.
In 2012, Geneva partnered with USAMRIID and the U.S. Army Medical Materiel Development Activity to launch a research program in response to NIAID’s call for a proof-of-concept study to develop a molecular vaccine for HFRS and to test the vaccine through Phase 1 clinical studies. The research, led by Dr. Shurtleff, in partnership with Drs. Connie Schmaljohn and Jay Hooper of USAMRIID, tested a combination DNA vaccine as a preventative measure against HFRS. Results demonstrated that this vaccine platform technology was safe and immunogenic, with evidence of cross-protection for the four target hantaviruses. Phase 2a clinical trials were conducted in 2020 under IND-14828 displaying an “unremarkable safety profile while inducing high-frequency immune responses against the target antigens.” In the manuscript, researchers stated, “Our studies provide a strong rationale for further large scale testing of these hantavirus vaccines to advance them toward licensure.”
Vaccines are an important part of public health, offering hope, and saving millions of lives each year. As vaccine research and development takes new directions through emerging knowledge about viral and bacterial diseases, Geneva is proud to press forward.
To learn more about Geneva’s infectious diseases research with a worldwide impact, please visit www.genevaUSA.org/infectious-diseases/.
HIGHLIGHTS
- COVID-19 has demonstrated the severity, complexity, and globalization of infectious disease outbreaks and the need for vaccines.
- Geneva is proud to collaborate on infectious diseases research at leading federal laboratories and military treatment facilities.
- COVID-19 and eight other life-threatening infectious diseases are on our radar including Ebola virus, dengue fever, chikunhunya virus, Lassa fever, Sudan virus, malaria, Marburg virus, and Hemorrhagic Fever with Renal Syndrome.


