20 October 2020
4D Bio3 Osteochondral Program Studying Cartilage Regeneration for Possible Treatment of Osteoarthritis
Joint diseases and conditions, such as post-traumatic osteoarthritis (PTOA), causes chronic pain and physical disability for millions of Americans. Due to the physical demands of military service, both active duty service members and veterans experience high rates of non-combat related disability related to PTOA. Arthritis is a leading cause of disability among military veterans and the second leading cause of medical discharge. Current solutions for joint diseases often result in chronic pain and reduced mobility.
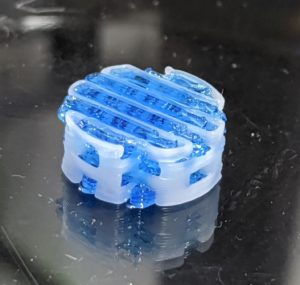
The intent of the 4D Bio3 Osteochondral program is to investigate various 3D print biomaterials and cells potentially for the treatment of osteoarthritis. Cartilage is an important tissue and mechanical interface between bones within joints. Repetitive injury or significant individual trauma can result in osteoarthritis and typically involves damage not only to the articular cartilage but also underlying bone and surrounding soft tissue. Recent progress in cartilage and bone tissue engineering has focused on developing strategies to regenerate, rather than replace, damaged or diseased bones and joints.
”3D printing in tissue engineering and regenerative medicine has expanded to allow a wide range of materials to be used simultaneously. This has allowed for osteochondral applications that more closely resemble the composition of the tissue compared to conventional fabrication techniques,” said Geneva Senior Research Scientist Joel Gaston.
The USU-4D Bio3: 4-Defense Biotechnology, Biomanufacturing, and Bioprinting Center (USU-4D Bio3 Center) is a collaboration between the Uniformed Services University and The Geneva Foundation.

”3D printing in tissue engineering and regenerative medicine has expanded to allow a wide range of materials to be used simultaneously. This has allowed for osteochondral applications that more closely resemble the composition of the tissue compared to conventional fabrication techniques,”
Joel Gaston, PhD, Geneva Senior Research Scientist


